Ototoxicity refers to the detrimental effects of certain medications on the auditory and vestibular systems, potentially leading to hearing loss, tinnitus, and balance disorders. As healthcare providers increasingly prescribe ototoxic medications, understanding and mitigating the associated risks has become crucial.
The World Health Organization estimates that over 5% of the global population needs rehabilitation for hearing loss. By 2050, this number could exceed 700 million. Hearing loss is a growing global health concern, with over 25% of individuals aged 60 and older affected.
This article will explore how providers can minimize ototoxicity risks through improved monitoring, education, and patient-centered care.
Understanding Ototoxicity
Ototoxicity is a primary contributor to acquired hearing loss globally, with early detection being crucial for reducing damage. The NIH indicates that various environmental factors, including aging, exposure to loud noises, and ototoxic medications contribute to acquired hearing loss.
Unfortunately, while ototoxicity testing is mandatory for drugs directly affecting the ear, many other therapeutic drugs do not undergo such testing. This has led to more than 200 ototoxic medications currently on the market.
Ototoxic medications can include aminoglycoside antibiotics, platinum-based chemotherapy drugs, loop diuretics, and even non-steroidal anti-inflammatory drugs (NSAIDs).
Symptoms of ototoxicity can vary, ranging from hearing loss, often beginning with difficulty hearing high-pitched sounds, to tinnitus (ringing or buzzing in the ears). Patients may also experience balance issues like dizziness or vertigo, or a sensation of fullness or pressure in the ears.
The Role of Healthcare Providers
Healthcare providers can assist patients in reducing the risks of ototoxicity by:
Proactive Monitoring
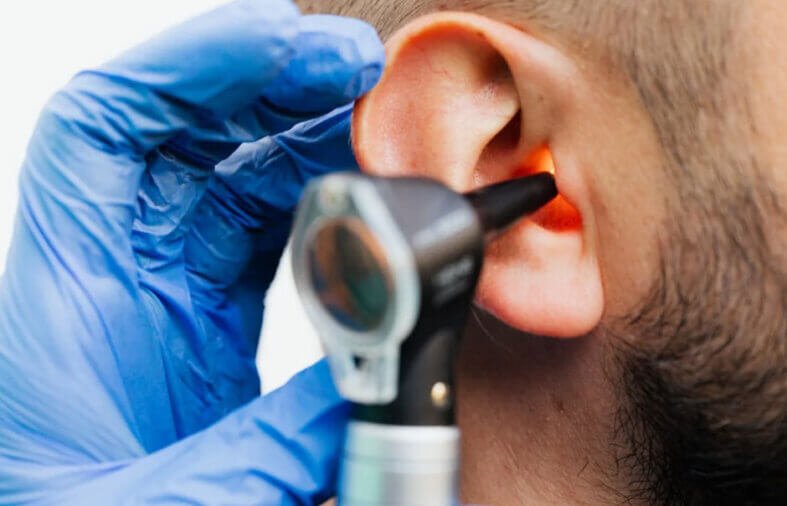
One of the most effective ways healthcare providers can minimize ototoxicity risks is through proactive monitoring. This involves regular audiological assessments before, during, and after exposure to ototoxic medications. By establishing a formal Ototoxicity Management (OtoM) program, providers can ensure that patients receive timely evaluations and interventions.
Audiologists can utilize various tools to monitor hearing function and detect early signs of ototoxicity. For example, Distortion Product Otoacoustic Emissions (DPOAE) testing can help identify changes in cochlear function that may indicate ototoxic damage.
Patient Education
According to Medical News Today, certain medications, including aminoglycosides like amikacin, neomycin, and tobramycin, carry a higher risk of tinnitus. Chemotherapy drugs, especially platinum-based ones, can also lead to hearing issues. Over-the-counter medications like aspirin, acetaminophen, and NSAIDs have been linked to tinnitus, particularly when used frequently.
A 2022 study showed that women who took these pain relievers regularly had an increased risk. Empowering patients with knowledge about medication side effects is essential for informed decision-making and effective health monitoring.
Multidisciplinary Approach
Implementing a multidisciplinary approach to care can enhance the management of patients at risk for ototoxicity. Collaboration among healthcare providers—including physicians, audiologists, pharmacists, and nurses—ensures comprehensive care.
For instance, pharmacists can play a critical role in reviewing medication regimens for potential interactions and advising on alternative therapies when appropriate. Regular communication among team members allows for timely referrals and coordinated care plans tailored to individual patient needs.
Policy Advocacy
Healthcare providers should advocate for policies that promote safe prescribing practices and enhance awareness of ototoxicity risks within healthcare settings. This includes supporting antibiotic stewardship programs aimed at reducing unnecessary prescriptions of aminoglycosides and other potentially harmful medications.
By advocating for guidelines that prioritize patient safety and informed consent regarding treatments, providers can contribute to a culture of safety.
Tepezza and Hearing Loss
Tepezza, a monoclonal antibody indicated for thyroid eye disease, has been associated with hearing loss as a potential side effect.
Initial studies indicated that approximately 10% of patients receiving Tepezza infusions experienced hearing-related side effects, according to TorHoerman Law. However, more recent research has shown that up to 65% of patients may experience hearing loss or related issues.
Before starting treatment, patients should be informed about the risk of hearing loss, and regular audiological evaluations should be conducted to detect any changes. If hearing loss is detected, a referral to an audiologist for further evaluation and management is essential.
The Tepezza lawsuit further emphasizes the drug’s potential risks. A lawsuit filed by an Oklahoma resident claims the drug caused irreversible hearing damage. The plaintiff claims that Horizon Pharmaceuticals did not sufficiently warn about the risk of permanent hearing loss, despite evidence from clinical studies.
The lawsuit seeks compensatory and punitive damages, holding the company accountable for its negligence in addressing known risks.
Frequently Asked Questions (FAQs)
How soon can ototoxicity develop?
Ototoxicity development varies. It can cause side effects as soon as you begin taking the medication, or even up to five years later. Some treatments may lead to delayed effects. This is why it’s essential to follow your provider’s recommendations for routine hearing exams to monitor your hearing over time.
How long can ototoxicity persist?
Ototoxicity can cause irreversible inner ear damage. While stopping the medication may not always be possible, your healthcare provider can adjust your treatment plan to prevent further damage. In such cases, a long-term care plan can be developed to manage symptoms, with risks discussed based on your diagnosis and prescription.
What steps should I take if I suspect I am experiencing ototoxicity?
If you suspect ototoxicity, contact your healthcare provider immediately. Report any symptoms, such as hearing loss, tinnitus, or balance issues. Your provider may conduct hearing tests and adjust your treatment plan accordingly. Early detection and immediate intervention are vital to prevent further damage and effectively manage symptoms.
Minimizing the risks associated with ototoxicity requires a proactive approach from healthcare providers. Through effective monitoring, patient education, multidisciplinary collaboration, and policy advocacy, providers can significantly reduce the incidence of hearing loss.
As awareness of these issues continues to grow—especially concerning drugs like Tepezza—healthcare providers must prioritize auditory health as an integral component of patient care.